There be Dragons - An Airway Adventure
This is a written version of a presentation by Dr Andrew Weatherall for a Paediatric Emergency Medicine Update. The brief was to cover as much as possible about the paediatric airway in an ED context.
The aim of this thing is very simple: to cover all there could possibly be to know about managing the paediatric airway in the Emergency Department in a pretty short bit of time. Or not, of course. If it was that easy to cover I’d be telling everyone that the subspecialty of paediatric anaesthesia wouldn’t really be a thing.
What can be done in a little short bit is a revisit of things most of us know because sometimes the important thing is to take up some time and space to look at things slightly differently.
So let’s go on a quest. A quest to conquer the airway version of a dragon – something not seen that often and potentially a bit scary. Look, it might be a small dragon.
I guess this makes me the Quest Master (look, I’d go with Dungeon Master but there would probably be some sort of copyright issue there, I don’t know).
Of course any quest needs heroes which means we need to introduce some characters.
Choose your players
The Characters
Each character hopefully brings some special skills to the table. They are, in no particular order:
The Engineer – who is good with their hands and getting practical stuff done.
The Master Toolsmith – skilled in the acquisition and selection of things that are required.
The Philosopher – the philosopher is particularly good at thinking and thinking about thinking.
The Butcher – good with a knife and OK with the sight of blood.
Oh, and there will be one other character who will only appear as an evil, disembodied laugh in your consciousness. But more of that later.
And now … The Quest
The local health facility in The Village, which actually services almost all the kids needing serious care locally, is going through challenging times. Forced underground by extensive renovation and rebuilding works to “facilitate better health experiences” and left short-staffed by unanticipated entirely predictable surges in demand, it draws on people who supplement their professional lives with entirely different jobs. This is what brings together an engineer, a master of tools, a philosopher and a butcher.
While on a break and bonding over war stories and some non-alcoholic mead the heroes are approached by the triage nurse. An 18-month-old patient with a background of trisomy 21 has arrived after being hit by a bike moving at high speed in the park. The ambulance called in that they had an observed reduced level of consciousness for 5 minutes, woke up a bit but then had some twitching activity and a vomit.
Now that they have arrived, the patient is agitated and a bit ‘all over the place’. Also, a bit of blood has been noted around the head and mouth and they currently have saturations of 91%. The triage nurse asks the team to assess and manage the patient, making sure to utter trigger words relevant to a noble airway quest,
“He’s heading for a tube.”
The First Question
The first question I had as QuestMaster(TM) was “which airway in the emergency department should we think of as difficult?”
Happily I only need to prepare for one answer kind of - ‘every airway in the emergency department is difficult’.
Now I should say up front that an issue with a lot of the literature is that the focus is all on intubation, when airway management is actually about being excellent with every step of airway management (supporting the native airway, face-mask ventilation, supraglottic airway management, intubation and readiness for front of neck access) to ensure continuous optimised oxygenation (and hopefully ventilation).
But putting that snorkel in gets the literature so we’ll have to accept those limits a little.
Across plenty of the ED-based papers they report on First Pass Success (FPS) for intubation. You can see why. First pass success is really easy to measure. It’s a binary thing. And there is some evidence supporting the fact that with more attempts come more complications and that is not good for patients. But we should keep in mind the goal is ‘airway management that optimises oxygenation’.
Anyway, across the FPS rates you see are in the 60%-90% range are pretty common (and plenty of those are at the lower end). And to give some context the evidence from other situations is that in more elective situations paediatric airway management generally goes well.
One useful study thanks to pretty big numbers is the APRICOT study (sigh, study mnemonics). This is a pretty epic bit of work where the researchers managed to capture data from every anaesthetic in 261 hospitals across Europe for a 2 week window. That left them with 31024 datasets to look at across 30874 patients (they started with 31127 but some patients had awake regional anaesthesia).
In a subsequent analysis of that whole dataset there were was a total of 11 failed intubations (in 13671 intubations). And there were no situations where patients could not be intubated and also could not be oxygenated it seems. That is pretty reassuring when it comes to the general patient wandering off the street (inclusive of those coming for emergency surgery).
So what might be different in ED?
One factor is probably numbers.
This is demonstrated quite well by a paper put out there by Long, Sabato and Babl back in 2014. A bit of time has passed but not so much that the reality described is that removed from now.
They looked at all the emergency department intubations happening in a busy (and very good) tertiary paediatrics hospital across a year. This particular place sees around 82000 patients across any 12-months.
They were left with 71 intubations to describe.
That is not many intubations. Even less when you consider for those intubations, the initial intubator was an ED specialist in 17 cases, the ED Fellow in 6, and the ED registrar in 22. So 63% of all of the intubations initially had someone from the ED doing the work. When you just think about the specialists they took the airway lead on 24%.
And an ED Fellow intubated a patient once every 2 months. It probably wasn’t the same Fellow.
And this is a problem referenced in this paper which seeks to tackle the question of how ED Fellow intubation performance changes over time.
Their answer - it doesn’t obviously progress hugely over 3 years.
And they highlight a similar issue to that raised by the Melbourne results.
The level of exposure matters.
How do you either acquire skills or maintain skills when only 71 of those procedures are required in a year and there are a lot of people working in your joint?
Before we even get to the possibility that the patients may actually be sick when they need an emergency intubation or any other factors that might influence airway management, the reality of doing a pretty serious intervention while getting irregular practice already makes airway management difficult.
Now it’s worth noting that the same authorship group who published that ‘ED over a year’ work have done some subsequent work showing that institution of standardised processes and education can result in improved performance.
But it remains the reality that opportunities to manage paeds airways in the ED are infrequent. And that’s a reality to wrestle with.
A Closer Look
So if we have to deal with that reality maybe we can add something about assessment. There are a variety of ways that have been described to assess the possibility of a difficult intubation in the ED.
The LEMON approach (Look, Evaluate, Mouth Opening, Obstructions (like swelling, saliva, blood, fractures, foreign bodies or masses etc) and Neck (movement and anatomy)) has been around for a while now though that pesky bit about checking the Mallampati score is not done in kids enough to be super useful.
When life makes you consider LEMON it is not actually time to think about making lemonade.
That led to the modified LEMON approach (where it becomes Look externally, Evaluate 3-3-2 rule, Obstructed airway, Neck mobility) but that still does not seem that well validated with one relatively recent paper suggesting that when it comes to predicting a difficult airway the sensitivity is around 41%, specificity around 73% and the positive predictive value a massive 9%.
It might be though that if you add consideration of prior airway pathology you might get to a pretty solid evaluation of difficult intubation - Galve-Navarro et al have published a little work suggesting that in paediatric patients if there is no history of airway pathology 95.14% of patients will be successfully intubated. That’s at least a little encouraging.
Really with all of these suggestions thought there are issues.
The first one is that issue of a focus only on intubation, not all of airway management. Like everything else, we should be thinking about assessment relevant to all of the techniques.
And then there a second issue one is they don’t consider the challenges of physiology. Not every difficult airway is about anatomy and gear. The challenges of an ill patient with compromised reserve and a tendency to rapid desaturation or haemodynamic instability might be the actual issue.
This makes the more recently developed HEAVEN criteria a little appealing. This particular mnemonic stands for:
Hypoxaemia (< 93% {assuming does not usually have low saturations} at the start of initial laryngoscopy.
Extremes of size (< 8 yo or clinical obesity)
Anatomical challenge (trauma, mass, swelling, foreign body or structural abnormality limiting laryngoscopy view)
Vomit/blood/fluid (in the oropharynx)
Exsanguination
Neck mobility.
And it comes with some validation. In work published in 2022, Tan et al. suggested that presence of any HEAVEN criterion was associated with a lower first pass success rate, though the strongest association was with anatomical challenge. Presence of hypoxaemia or Vomit/blood/fluid were associated with airway complications.
This makes it all feel like we’re getting closer to useful assessment criteria when it comes to the airway, as long as we also consider all the available airway management techniques in this context.
That said, we’re still missing a few other things that influence our ability to manage the airway and that should be part of our evaluation.
Those factors have previously had me teaching a slightly different mnemonic for assessing an airway situation:
where the categories are:
Patient - all the things that are always there at patient baseline that might make it difficult (known difficult intubation, airway pathology, syndromes, prior neck or jaw surgery etc etc). It’s an easy way to incorporate a couple of key extra points - the patient being under 1 y.o. and under 10 kg also definitely increases the likelihood of difficulty.
Acute - all the acute things that have added difficulty to the baseline (blood, respiratory disease, haemodynamic instability, increased oxygen consumption, abdominal distension etc etc).
Scenario - what is your scenario when you come to manage the airway? During the day at a big hospital? The middle of the night in a remote ward in a small hospital? The scenario itself can add a huge degree of difficulty (and certainly does in ED).
Team - airway management is a team sport. I even made 4 people join a team of characters on a quest. To properly evaluate an airway management situation, it is worth assessing the experience, readiness and familiarity of the team.
Which is why it’s just as well we have a Philosopher to consider all the team dynamics and thinking about thinking stuff.
And if I could distil all the things Philosophers definitely always say about paediatric airways in the ED it would include the following:
“Treating all airways in ED as difficult makes sense because the real world evidence suggests that good ED teams find them difficult. Plus if you set up like the situation is going to be difficult, you’re ahead of the game for the greater number of times when it’s not.”
Quests are boring if you allow too much latitude of course. So for now, lets condense all the clever talk into something that is very often right – the triage nurse was correct.
Let’s Pause Time
Now in any good quest there is usually scope for the use of special items. For this quest the first special item is the “FirstNet Magical Device of Time Relativity” capable of making time speed up, slow down or become entirely unhinged from reality in the manner of all good computer systems.
So in this quest our heroes have the opportunity to suspend time so they can check the old books, in particular “The Book of Ye Olde Knowledge and Understandings”. This is a chance for our heroes to make sure that some simple things about the paediatric airway and its management were understood equally by all. Why start something difficult without brushing up?
In particular it seems sensible to double check that the things we all knew about blades, rings and cuffs are up to date.
Except the problem with old books is they need updating, and sometimes the best bits are the helpful scrawls in the margins where people have provided newer info.
The outside alone won’t cut it.
Maybe it’s worth starting with the ring (that’s the cricoid ring) and the cuff (the one on the tube) because they are pretty linked.
Since what feels like the dawn of time we’ve been told that children have a conical airway and the cricoid ring is the narrowest part of the airway.
Except it’s not.
Well, at least, it’s not that simple. If it was simple people wouldn’t get so worked up about it. And wow do they get worked up about it.
The classic descriptions of paediatric airway anatomy that push in this direction seem to have started mostly with cadaveric studies (not even the whole airway, just removed airways) from small people using techniques available at the time (e.g. plaster casting) but not so obviously linked to the natural state.
Which was what you had to do.
But the thing is now we have studies that have used MRI, CT and airway endoscopy and the picture looks, on balance to be a bit more subtle.
The cricoid ring is quite narrow. And it is definitely the one completely rigid thing in the airway so that’s really important.
But in the native state the space between the vocal cords would be narrower (though not such an issue when intubating). And interestingly the subglottis seems to be the most crowded area (although the A-P diameter at the subglottic region is greater than the cricoid, the lateral dimension is smaller). That said, that bit is also distensible.
So the subglottis is anatomically narrower, but functionally the cricoid really counts.
Now there are people out there still very committed to cadavers and who seem less worried about the issues of whether or not cadaveric tissues are actually the same as those in an alive child.
But to be honest that doesn’t appear to make a heap of sense. Evidence from actual living people seems quite useful.
This is all relevant to the cuff. I set it up like cuffed tubes still carry some controversy. But realistically, they are chosen more and more because they offer better ventilation characteristics.
However thanks to the functional importance of the cricoid ring and how close everything is between cords, subglottic and that one rigid structure, the choice of endotracheal tube (ETT) really matters.
At the moment it’s really the Microcuff ETT that deals best with the challenges inherent in the smaller person airway by having a cuff that is closer to the tip of the ETT. Even with this accommodation it is quite possible to have the cuff inflated close to or in the cricoid ring and that likely increases the risk of airway injury created by your tube, even if using a cuff pressure manometer and reaping the benefit of the very delicate low volume/high pressure cuff.
So for all age ranges, maybe except children under 3 kg (and sometimes even in them), cuffed ETTs tend to be preferred, particularly with evidence of no increase in complications in retrospective studies of the under 7s or under 5 kg tikes.
Cuffed tubes are a great bit of equipment. But a great bit of equipment can still cause problems if used badly.
Of course to get it there we’re probably going to use a laryngoscope. And 10 years ago a lot of the chat would have been about straight vs curved blades. And that would be a chat about how straight vs curved is less important than ‘did I use the right technique for that style of blade’ because they are both pretty successful devices in most normal kids.
The more up to date chat would be about videolaryngoscopy (VL) vs direct laryngoscopy (DL).
And the sands are definitely shifting towards VL for all the obvious reasons. It seems like the view is more likely to be there and it offers the benefit of everyone in the room having a view.
No brainer, right?
Well, ¯\_(ツ)_/¯
The best summary of the current state of play is actually probably from a recent editorial by Disma et al where the basic sentiment is ‘current evidence does not support routine VL outside neonates’.
Time and time again the message appears to be that for all comers, you tend to achieve a better visualisation but often a longer time to intubation. First pass success (FPS) is often not that different or only higher in neonates.
In fact, you’d expect VL to really show a benefit in the ‘limited neck mobility’ group (as in C-spine precautions etc etc). Even there in a study by Khanam et al the FPS was 79.8% with VL and 75.7% with DL (not reaching significance) and with no difference in adverse events.
The further disappointing thing in the literature is that there isn’t as much of a focus on whether the patients had a different experience of oxygenation through the intubation. You’d think it would be front and centre. Almost invariably it appears studies are not powered to look at that.
Oh, and what about hyperangulated blades vs standard profile? Well, there is some evidence from one of those many PeDI papers that standard profile VL has a higher success rate in infants under 5 kg presenting difficult airway challenges than a Glidescope (which is, by its nature, hyperangulated). And that might be reassuring because the technique for any hyperangulated blade is a bit different and needs practice, whereas a standard profile blade that happens to be VL probably allows the occasional paediatric intubator to draw on their background skills grabbed from adults.
At the end of the day, you’re likely to choose VL. But if you can’t it’s not a major breach of gold standard evidence. And either way a focus on how you’ll maintain oxygenation throughout is critical.
Phew. Maybe we should let the clock start again. But let’s make a very quick and entirely imaginary trip to the armoury (which will not be at all discussed here because once you get a Master Toolsmith amongst the equipment we risk an all day side quest) and we best move on to making plans.
Just a note to say that if you can find a Device of Time Relativity to pause the action at your work at will, it is a worthwhile investment. Bit weird that this one looks more modern than the rest of the quest.
Best Laid Plans
In the context of this quest, a key point is reached when you ready the field of battle.
OK, that’s a little aggressive for a paediatric airway thing.
Maybe a key point is reached when you get ready to go about your work.
And in this context let’s consider 4 key areas to cover:
The space – think about the layout of your working space. How much access do you have around the treatment area? Are the things you need logically laid out and easy to get to? Are the things you need right now closest to you? Is there anything you can optimise?
The bed – I mention this one specifically because so often people seem to be stuck on the idea that the bed must be absolutely flat for airway instrumentation. Why? Have a really good think about whether having the patient sitting up at least a little might be a better option for functional residual capacity and respiratory management.
The kit – you’ve chosen it but have you double checked it worked and briefed what you’ll do?
The people – the agreement of most seemed to be that you’d probably want four people ideally. One to manage the drugs, one for doing the technical stuff, one as the assistant and one keeping an eye on the big picture. Of course if you’ve trained for it you can do it with less but we’re talking about optimising things where we’ve assumed a difficult airway.
After all that we still need to lay out a plan. Now there are lots of ways to do that and an excursion into checklist territory would defeat even the magic time-stopping clock and have us here until next year.
What is critical is that the approach to planning includes the whole team, is fully briefed, and ensures that everyone shares the same mental model for what will happen. The best people in the world can’t do a job well if they don’t know what the job is. So briefing the plan properly is a major part of any success.
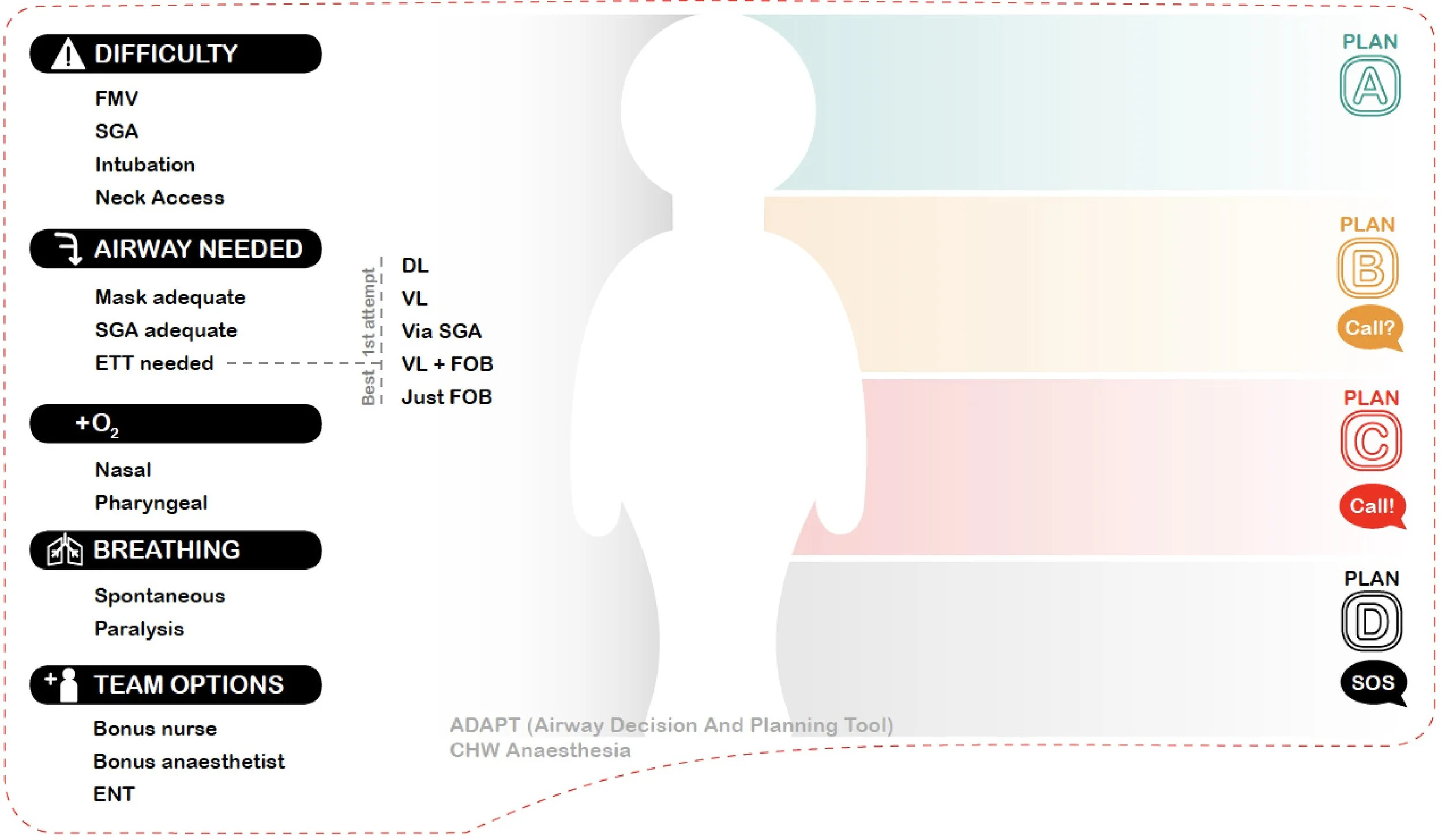
Locally we have the Airway Decision and Planning Tool which is laid out to allow a team to come together to highlight what will be difficult, what airway they need (mostly pre-selected for ED), what will offer the best first attempt for this team, any plans for additional oxygen, paralysed or not and whether to call for bonus helpers (an extra feels like a third wheel and a bonus is always great).
It also offers scope for the team to lay out the plan A/B/C/D that they will work through in their context with the patient in front of them with their skillset.
It’s a slightly different approach to the rigid Plan A is this tube thing and plan B is always a supraglottic etc etc. There are pros and cons to both. The most important thing is that the plan is fully understood by all in a way that everyone can efficiently help to act upon it (and feel empowered to step in if things drift).
It’s just one way but lets the team own the plan
A Pause for Some Fresh Air
Just before it gets really tense and the action starts, it seems worth mentioning the fresh air bit - nasal prongs or apnoeic oxygenation.
The story of apnoeic oxygenation is really interesting. When it hit the scene there was a heap of really positive and promising things about it. And there were lots of people (and still are lots of people) who are super committed to it.
The thing is it’s worth noting that there is not a heap of evidence that suggests it is more successful at preventing desaturation than other approaches to maintaining oxygenation (not that there have really been direct comparisons of different approaches).
Certainly for kids the picture is mixed and maybe that’s because the logistics of getting the nasal prongs situated for kids after breaking the face-mask seal suck, or if you try to do it before pre-oxygenation you don’t maintain the seal well enough.
But it’s definitely not the sort of thing your local apothecary would describe as a ‘cure-all’.
What counts the most is good pre-oxygenation. That takes time and a good seal (and probably gently bagging through the apnoeic phase).
Applying nasal prongs to sit under the mask isn’t necessarily going to help preoxygenation. There are works in the literature suggest that an optimised patient (i.e. elective induction of anaesthesia, muscle relaxant on board after pre-oxygenation, with the airway held open and nasal prongs applied or not) probably has an extension of the time to desaturation. That’s not rapid sequence intubation though.
More recently the HAMSTER study suggested humidified high flow nasal oxygen was not superior to oxygen delivered to the pharynx via other means in terms of avoiding desaturation episodes during airway surgery (a different setting but still interesting).
But perhaps the most interesting recent study is by George et al where the intention-to-treat analysis included 476 patients had nasal high flow oxygen vs 474 who had standard care in critical care intubations. This was in an RCT setting. On the ‘analysed as per the group they were put in’ numbers (modified ITT), there was no significant difference in hypoxaemic events (12.8% for NHF and 16.2% for standard care but the adjusted odds ratio 97.5% CI stretched from 0.46-1.18).
The first pass success rate with no desaturation was also no different.
A key wrinkle in this study was that in 45 patients in the nasal high flow group, the involved clinician either didn’t apply it or took it off. And while the authors did a ‘they received what we intended’ analysis (a planned per protocol) that did show a difference in hypoxaemia rates, the fact remains that 45 times, the senior clinician thought the best option was to take the nasal high flow away.
Could they not get it on right? Was it causing issues? Did it delay them getting on with things?
We can’t know. But it seems important to recognise that in the real world, it’s not always actually going to stay on and there is some logistics factor to keep in mind.
At the least it should make us look at barriers to use. Or consider other ways to maintain oxygenation.
Just a thought while we take a few breaths of fresh air.
And of course, finally, it’s time to roll the dice.
As for any good quest, all of our fates come down to the dice.
You can roll with advantage
Now that the adventurers have put down their non-alcoholic mead, come together, assessed a patient, frozen time, read some books, cross-referenced feng shui principles to arrange the space and kit and made an amazing plan, it seems only fair to draw on the person who gets things done, The Engineer, to roll with advantage.
However who needs advantage when the Engineer will definitely roll a 19!
This, happily, is a very good number to roll (although anything over 3 would do the job because more often than not things will go fine).
The preoxygenation was brilliant, the medications were well chosen, the laryngoscopy was not at all an issue and the endotracheal tube was placed without any fuss at all.
Success! \o/
Of course at that moment, our fifth player enters in the form of an ominous and evil laugh…
This is of course The Evil Necromancer of the Executive Suite who, armed only with a clipboard and an email account, is capable of inflicting multiple contradictory realities on hardworking clinicians at any moment.
So just as our heroes have triumphed, they find themselves back at the point of preoxygenation, ready to roll again.
Roll 2
The Engineer takes up the 20-sided solid of destiny again and rolls. And they are unsuccessful. Do not ask what they rolled. They are just unsuccessful because if you’re the QuestMaster(TM) you get to say so.
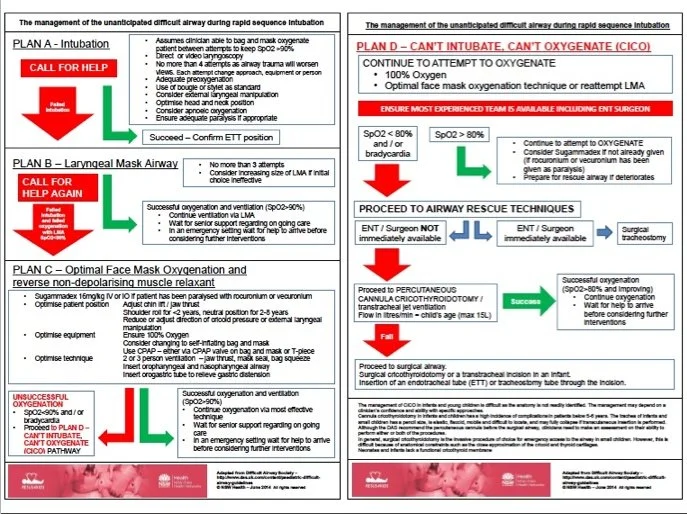
Which means that now they need to think about the algorithm you need when you don’t get the tube in. And maybe everyone is familiar with something like this….
The point here is there is lots of good stuff but it’s very busy once you’re in a tough spot. This is the nature of almost any of the airway schemes you could put up.
This is a good algorithm with lots of sensible things on it. It’s also one that might be hard to work through in the heat of battle with an airway dragon. It’s one to have tried to digest beforehand.
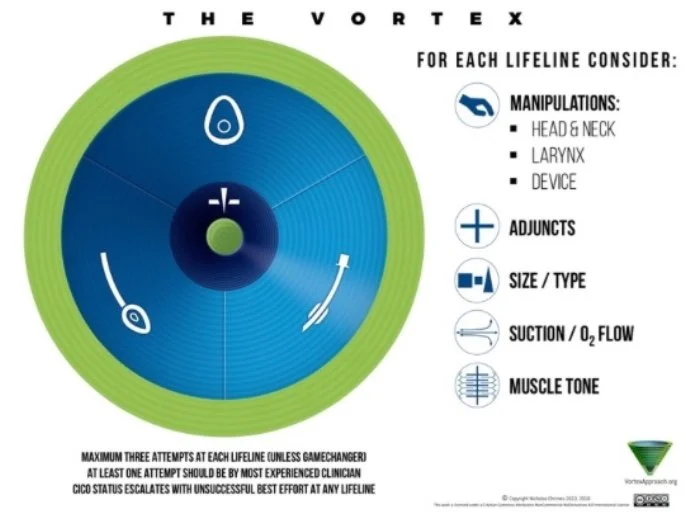
If you turn to The Philosopher who thinks about thinking they will no doubt agree that at times of stress it’s pretty useful to be able to reduce our thinking to simple things. Things that we can visualise easily and know what they mean.
I personally quite like the simple mental overlay offered by the Vortex Approach.
Simple. 3 techniques. Keep moving. Find safety.
Whichever mental pathway they used to get there, let’s say The Engineer asked the Master Toolsmith for a supraglottic airway and they reach a point of safety with successful oxygenation. \o/
Success!
But then the evil laugh of The Evil Necromancer of the Executive Suite rings out again.
The team are back at the point where preoxygenation was just ending…
Rolls 3, 4, and 5
And now it’s getting exciting. And not just because I put an Oxford comma in that heading.
This time all the rolls for placing an endotracheal tube, rescue with face-mask ventilation and the step for insertion of a supraglottic airway come up with the wrong number. Look, it doesn’t matter which wrong number they are all just the wrong number.
The time has came for a player who you can assume has offered many words but not many actions to step forward. It is time for The Butcher.
At this point in the scenario it is time to chat through different front of neck access techniques. Actually even before this it was time to mention that CICO situations in kids are really super rare.
How rare?
Well, You can also look at stuff from the PeDI registry, a specific multi-institution study looking at difficult airway cases. It’s defined in that registry as kids who have difficult laryngeal exposure (think Cormack and Lehane 3+), those in whom conventional direct laryngoscopy is impossible, children with prior failed direct laryngoscopy within 6 months, and those where alternate techniques were chosen.
In that super difficult group there was a total of around 2% of patients (of their 1018) who had some form of surgical airway. The other thing that matters though is that there were only 10 recorded cases where either face-mask ventilation or supraglottic insertion were impossible (and it’s hard to get a sense of whether there was overlap in those groups).
But those are difficult patients. Even more persuasive is the APRICOT study again. Across all those 30000+ anaesthetics they did not see a CICO situation.
So the chances of truly failing oxygenation seem incredibly low, and if the planning has been done and support summoned then the chances of ending up at this part of the algorithm in the ED really seems incredibly low.
Still, preparedness matters in any village health facility.
The most important things to note about front of neck access in kids would be:
The suggested techniques in different age groups are based on consensus and that consensus is invariably hard for people to arrive at. Plenty of algorithms suggest cannula cricothyroidotomy in the under 8s, but I’ve seen some paediatric anaesthetists publish opinions that those kids should definitely have a scalpel technique deployed. Even recently a group suggested the surgical approach for all (thought they suggested you’d start with a laryngeal handshake manoeuvre which, given the compressibility of the airway in small people seems just not feasible in the way it is in an adult).
Either way the anatomy can be hard to define and there are those who suggest abandoning all pretext of finding the cricothyroid membrane and just aim for trachea. Access to the area can also be difficult just because it’s a tight little spot.And in smaller kids the trachea is very pliable and it is very easy to produce posterior tracheal wall injury or even puncture. There are no good options here.
The best bet is therefore not getting to that point.
Perhaps the best thing to offer is a solid review and this one by Sabato hits the mark and the only evidence that has popped up since then are a few more rabbit model animal things. That one ends up concluding that it is reasonable to consider the cannula technique in the under 8s. But also not to spend long on it and be mindful of the risks. If that’s what you choose you have 30 seconds to find the midline and get it done. Or move on.
As a general point on this if you are looking at front of neck access there are a few practice points worth contemplating:
It’s worth continuing to attempt to provide oxygen from the top end.
Prepare early – briefing it before everything is a good start and after that first challenging attempt ideally someone should be starting to get ready with just that job in mind.
That person has to mentally focus only on managing access from the neck.
After that it’s important to slow things down a little rather than try to be super fast, talk out loud through what you’re doing and involve the team. You might as well share that stress.
Amazingly in this case with Roll 6 The Butcher deploys a cannula with excellent technique, hooks up to an appropriate device for provision of oxygen without jetting ginormous pressures and achieves oxygenation just as those summoned by that pesky magic rock turn up.
Success! \o/
And this time The Evil Necromancer must be on a conference call because there is only silence.
Well until a mighty ‘Huzzah!’ from everyone involved in managing this particular paediatric airway.
Maybe now our heroes can share some of this mead that references some other thing that will never catch on.
Coda
The patient and their airway have been successfully managed. The team will retell their story, first to the other workers who will take over care of the patient and then in the parchment version of the patient record so others may hear tales of their noble quest.
They will recall that all paediatric airways could be considered difficult. They will write new books in which the useful things in the marginalia are actually just the things written in the books. They will teach people about knowing their equipment and set-up, briefing a well-drilled team, optimising their chances with each technique and the great joy to be found within the meditation of pre-oxygenation. They will talk about achieving clarity through simpler thinking at moments of stress.
And at the end of the shift they might just go and find some mead that isn’t labelled non-alcoholic. And even plan their next encounter with some other kind of dragon.
Some Light Reading
OK, that was a fair bit. But really to get the most out of anything (and help fix up any bits where you have a different perspective) it would be great to go and read some source literature. So, here’s a little light reading that was used to underpin the adventure.
First up, that analysis of the APRICOT study:
That great RCH ED intubation paper is here:
The ED Fellows performance trajectory over time paper is this one:
The HEAVEN criteria validation thing for kids is right here:
The validation paper for the modified LEMON criteria referenced is this one:
An explainer on PAST is linked right here.
Now, a little bit on anatomy and cricoids. There is so much out there that a pretty good starting point is actually the editorial by Peyton et al. It puts in context some of the recent anatomical stuff in cadavers with some clinical input. But I also have links here to the Isa paper based on the cadaver work, plus some other bits on anatomy .
Now, here are a few things looking at airway problems after use of a cuffed tube.
Now, how about VL/DL. Honestly, there is a bazillion papers here. Let’s go to the summary of the editorial:
That thing on use in limited neck mobility kids is this one:
The specific thing on standard profile VL vs the hyperangulated Glidescope in difficult airways in infants is right here:
A link to a quick explainer on the Airway Decision and Planning Tool is here.
The HAMSTER study thing (high flow nasal oxygen in a slightly different setting) is this one:
The more relevant RCT in critical care settings is this one:
Now, to CICO. Let’s start with a description of people arriving at algorithms just to note no one really knows what to do in kids:
The Sabato education review is good and pretty sensible. It doesn’t have the evidence from more recent rabbit models but the logic remains sound and it’s not particularly clear that the animal evidence really changes much compared to the summary here:
The more recent educational review is this one. Lots of good stuff in there and see if it persuades you on technique choices:
And if you got this far, you have earned a few moments of something entirely different. But perhaps it can also be about getting ready for a fight or something?
Here is an excellent thing from ‘Every Frame a Painting’ on the legendary nuance of Jackie Chan.